Personalized Approach
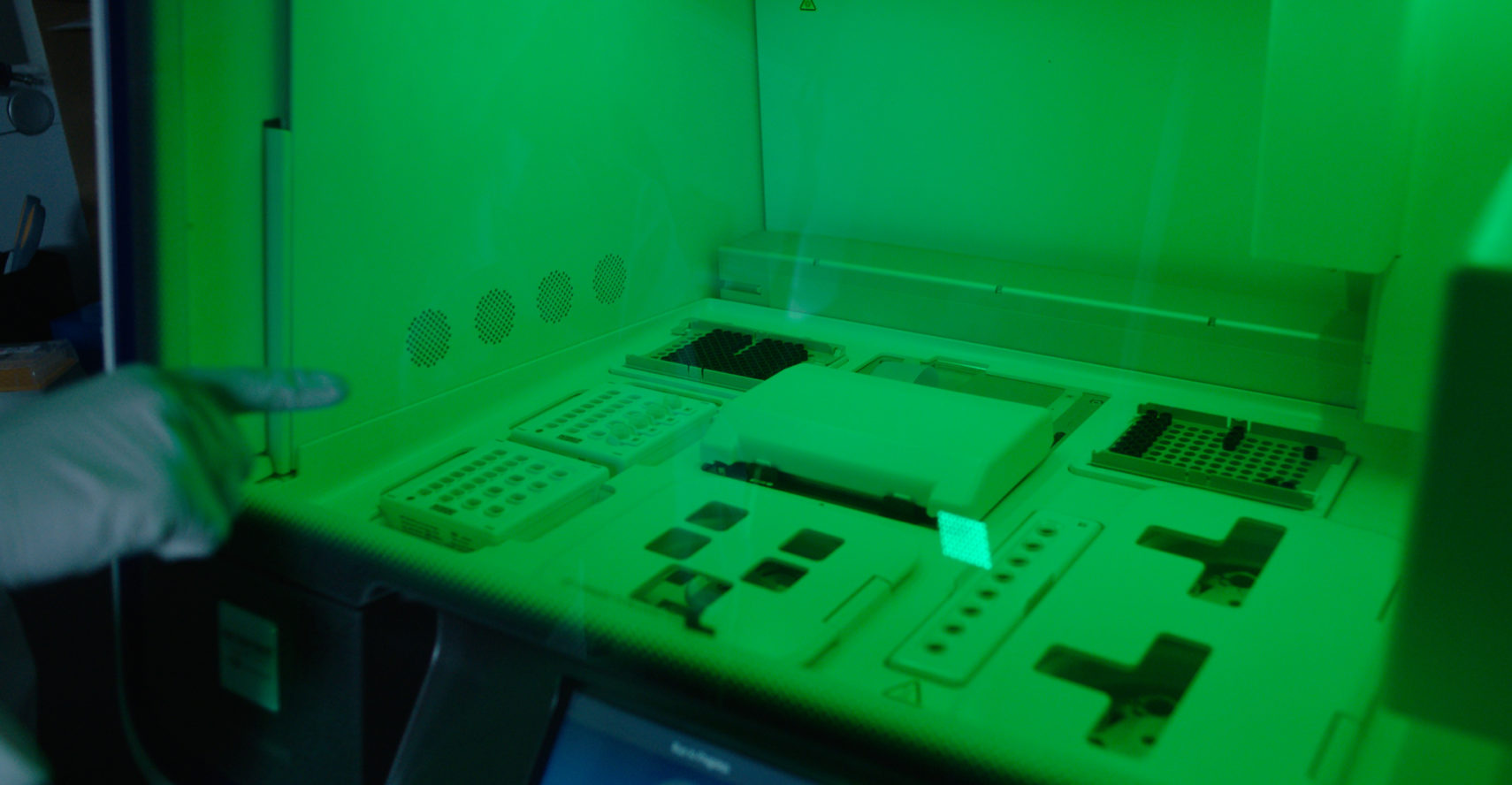
The future of cancer medicine relies on information about a patient’s unique genetic makeup and the composition of his or her specific cancer. This information is extremely helpful in selecting the best treatments for targeting specific genes and proteins responsible for cancer cell growth. Sentara continues to focus on precision medicine as a means to offer a more personalized and effective approach to cancer treatments.